At the conclusion of Part 1, I summarized how well I adhered to the antecedents of my hypothesis: no added sugar and more exercise. As I progressed through the physical protocol of my experiment, I also continued to research the chain of reasoning espoused by my GP.
A Big Fat Surprise
In addition to following the YouTube trail of Robert Lustig videos, I cracked open a book that had been sitting unopened on my shelf for some time, which I purchased after hearing Nina Teicholz interviewed by Tom Woods: The Big Fat Surprise. Although my GP had made no mention of fat as a problem in my diet, a quick check of the index – boy, do I love non-fiction books with a good index – I could see that LDL cholesterol was discussed substantially. So I dove in, and the murky, choppy sea into which I dove was indeed a surprise. Teicholz book is written more like a historical who-done-it, but with an abundance of footnotes and references. Infused with her own wry wit in the face of what can be conservatively described as disturbing subject matter, I can't recommend this book enough. There were many occasions while reading when I stopped to read a passage aloud so my partner could share my disbelief. A few examples include unreasonably broad claims and conclusions resting on the back of shoddy science; the intentional, eventually systematic, repression of science that disagreed with the diet-heart consensus; a low-fat diet recommended to a nation including women and children when it had only been clinically tested on adult men.
Indeed, Teicholz's tome, Lustig's lectures, other reading made it clear to me that there was a long tradition of dissent with the chain of reasoning that dietary fat causes high blood serum cholesterol, which in turn causes heart disease, and that cholesterol-suppressing medication was the first, best countermeasure. Well-constructed attacks on every piece of this argument exist.
There's a specific chain of reasoning that needed to be substantiated before I began taking statins, potentially for the rest of my life:
- If I have high LDL cholesterol (>130 mg/dL, especially >189 mg/dL), I am at greater risk of coronary artery disease (CAD).
- Atorvastatin/Lipitor reduces the risk of CAD.
- Taking Atorvastatin would increase my chances of living a longer, healthier life. (Reducing CAD risk alone isn't enough.)
That is, including minor side-effects, more serious adverse effects, and opportunity cost of $91/year, is taking atorvastatin the best way to increase my healthspan? (Hat tip to Ivor Cummins for this perfect neologism from the 1980s.) There are a few links in this chain; all must stand up to scrutiny. The sum must be better than other available options in overall value.
Claim: High LDL is Correlated with CAD
LDL is not the metric most strongly correlated with CAD. More strongly correlated measures include:
- triglyceride/HDL ratio - notice that this is available even in the simplest lipid panel that only measures total, HDL, triglycerides, and estimates LDL
- apoB/apoA‐I ratio
- large bouyant vs small desnse LDL
For triglyceride/HDL ratio, it's possible that the reason it's not more relied upon is that adverse-effect-free medications don't exist to modify either of these measures; lifestyle changes are required. For apoB/apoA-I, it's not a part of the currently commonplace blood lipid panel, and is therefore less accessible to your average general practicioner.
Moreover, "high LDL-C is inversely associated with mortality in most people over 60 years".
At best, LDL is at best a proxy measure; many people with "normal" LDL suffer heart attacks and many people with elevated LDL don't. Refinement of proxy metrics is both possible and desirable. Before blood lipid subfractions could be measured, total cholesterol was considered a usable proxy measure of CAD risk; today it's not considered alone. It's seems that enthusiasm for LDL is likely to fade, as well, as we've learned that the large, bouyant sub-subfraction of LDL is benign with respect to CAD, making the total LDL count misleading.
To summarize, before I'd even reached the end of my experiment, my enthusiasm for LDL as a metric to focus on had waned considerably.
Claim: Lipitor reduces LDL
Mark Twain said, "There are three kinds of lies: lies, damned lies, and statistics." Check out this early ad for atorvastatin:
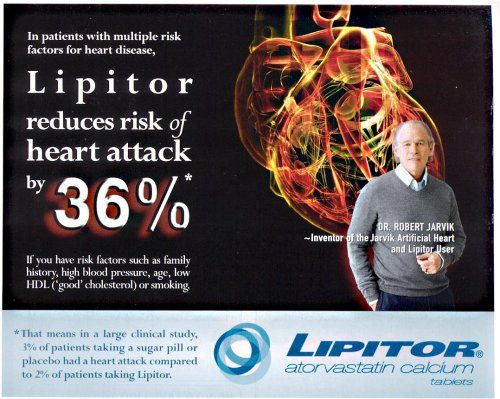
Impressive, isn't it? Be sure to read the fine print.
- atorvastatin reduces the relative risk of heart attack by 36%; it reduces the absolute risk by about 1%
- the relative risk reduction claim is limited to individuals with other heart attack risk factors
Using the American College of Cardiology risk calculator, I estimated my baseline risk of ASCVD at 1.8% over the next ten years, based on the preliminary blood test (on the basis of which the prescription was originally written). A 36% reduction means I could expect to reduce my chances of ASCVD over the next decade by 0.65% by taking atorvastatin every day.
Claim: Statins Probably Increase my Healthspan
Potential atorvastatin adverse and side effects include:
- skeletal, joint, and muscle weakness, ache, and pain
- increased insulin resistance and chance of Type 2 Diabetes or "pre-diabetes"
The former might be dismissed as an irritation, I can't help but think that it would discourage activity and exercise, one of the best things I can do to mitigate my risk of CAD. (Although it's purely anecdotal, one friend who had taken atorvastatin suffered from "serious" muscle aches and pains, and encouraged me to investigate other options thoroughly.)
The latter, insulin resistance and type 2 diabetes, is serious, as it's associated with many health problems and mortality causes separate from CAD.
The opportunity cost of taking the medication daily and purchasing it quarterly is important, too. That is, could I spend that time and money in a different way that would reduce my risk (of mortality, not just CAD) more than 0.65% over ten years?
Measure Twice
A friend of mine works for EverlyWell, and because I think they have a neat suite of mail-order testing products, I decided to utilize their Cholestoral & Lipids Test at the same time as the blood draw for my follow up test.
I fasted overnight, visited my doctor's office to have blood drawn, drove home and pricked my finger for the EverlyWell test less than an hour later, with no food or drink consumed between, and no significant physical activity. In a few days, I had my pair of results:
| EverlyWell | Quest | |
|---|---|---|
| total | 245 | 279 |
| HDL | 50 | 57 |
| LDL | 132* | 204† |
| triglycerides | 63 | 70 |
all measurements in mg/dL
* measured directly
† estimated via Martin-Hopkins method
WHAT THE @#$?! Not only do these results disagree significantly regarding LDL, but starting with the baseline measurement in November (186) they indicate changes in opposite directions!
Comments powered by Talkyard.